Are Prior Authorizations Stealing 2 Business Days? Here’s the Fix
Every spring, Physicians Practice surveys clinics and health groups to uncover what’s truly keeping their administrators up at night. The 2025 results are in—and the message is clear:
Prior authorizations are the top threat to practice efficiency.
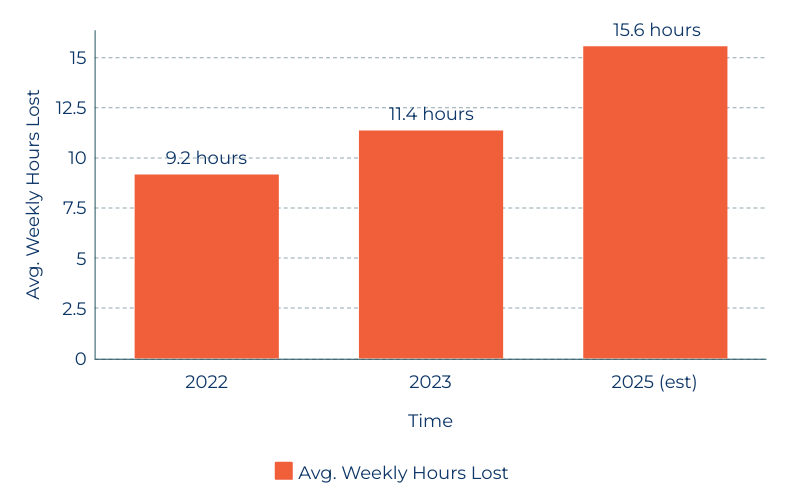
The Rising Tide of Prior Authorization Delays
More than half of practices (58%) cited “dealing with payers” as their number one pain point—especially when it comes to burdensome prior authorizations. These slow, repetitive tasks aren’t just an inconvenience—they’re consuming up to two full business days of staff time each week.
According to the American Medical Association’s April 2025 survey:
The average physician now handles 39 authorization requests per week
That workload alone drains almost 16 hours—nearly 2 full workdays
And worse, the policy solutions in Washington have yet to materialize
A Perfect Storm: Staffing, Cost, and Burnout
Staffing shortages came in a close second on the survey at 56%. MAs, coders, and even physicians remain hard to hire and even harder to retain. MGMA data shows 70% of groups are still battling turnover, with one-third reporting it’s actually getting worse.
Meanwhile, the cost crunch continues. Inflation may be cooling elsewhere, but not for medical practices. Medicare’s latest reimbursement cut (2.83% in January 2025) marks the fifth consecutive drop—piling pressure on practices already paying more for staff, supplies, and rent.
Then there’s the admin fatigue. From EHR overload to denied claims and excessive documentation, nearly 40% of clinicians say “administrative burden” is a top daily challenge. AI-powered tech promises relief, but only 2% of practices say they’re prioritizing it this year.
Time Lost to Prior Authorizations (2022–2025)
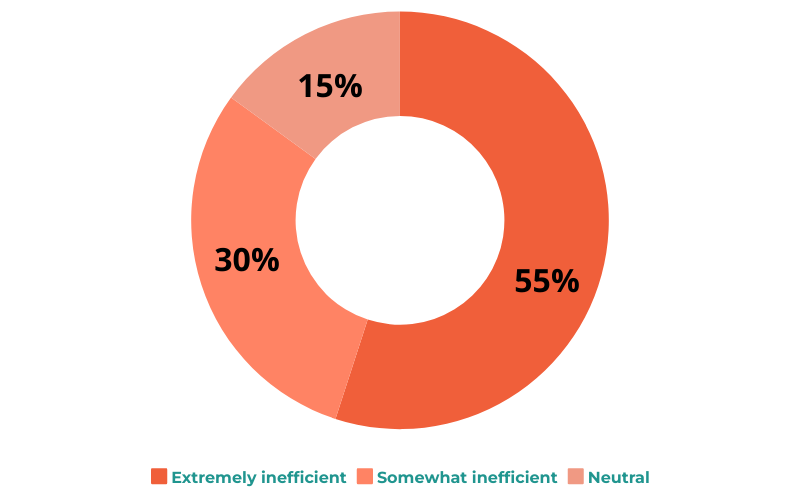
Satisfaction with Prior Authorization Process
The Fix: Remote Care Monitoring (RCM) That Does More Than Monitor
Amid all this pressure, one solution is standing out: Remote Care Monitoring.
Originally used to track vitals and symptoms between visits, modern RCM platforms now serve a broader purpose—streamlining communication, automating documentation, and even reducing the number of unnecessary prior authorizations.
Here’s how forward-thinking practices are using RCM to reclaim control:
✅ Reduce Prior Authorizations
By monitoring chronic conditions remotely and submitting automatic reports, many approvals become proactive rather than reactive—reducing denials and last-minute scrambles.
✅ Generate Reimbursable Revenue
RCM services like RPM (Remote Patient Monitoring) and CCM (Chronic Care Management) are Medicare-reimbursed, helping practices offset declining in-person visit margins.
✅ Relieve Staff Workloads
Remote teams and automated systems handle check-ins, documentation, and tracking—giving back hours of time to short-staffed teams.
✅ Improve Patient Engagement
Patients with access to remote tools report better adherence, fewer ER visits, and higher satisfaction—creating a positive loop that reduces administrative back-and-forth.
One small shift—offloading routine tasks to remote care tools—can free up 16+ hours per week and help your team refocus on what really matters.
Smart Practices Aren’t Waiting for Reform—They’re Rebuilding Systems
Congress may eventually address the growing administrative load on providers. But innovative practices aren’t waiting.
They’re:
Automating redundant workflows
Hiring remote care coordinators
Building hybrid models that scale capacity without burnout
Want to Reclaim Lost Time in Your Practice?
You don’t have to overhaul everything at once. A small shift to remote monitoring workflows can make a measurable difference in both revenue and retention.
📅 Start with a short strategy call.
Let’s explore how your practice can use RCM to ease the burden of prior authorizations and lighten your staff’s load.
