What Every Practice Got Wrong About New Tech (And How to Avoid It)
In recent years, healthcare organizations have poured billions into technology upgrades—from digital front doors to AI-based clinical tools. Yet, instead of improving outcomes and streamlining workflows, many of these systems have created confusion, burnout, and inefficiency.
If you’ve ever wondered why your expensive patient portal isn’t being used… or why your EHR upgrade left your staff frustrated, you’re not alone.
Let’s break down where practices are going wrong—and how to avoid the same fate.
💡 The False Promise of “Innovation”
Many practices fall into the trap of assuming that new technology automatically means better care. Vendors promise time savings, patient loyalty, and seamless integration—but without user-centered design and real-time adaptability, these tools become just another checkbox.
Take this real-world insight from recent data:
📉 Provider Satisfaction After Tech Implementation
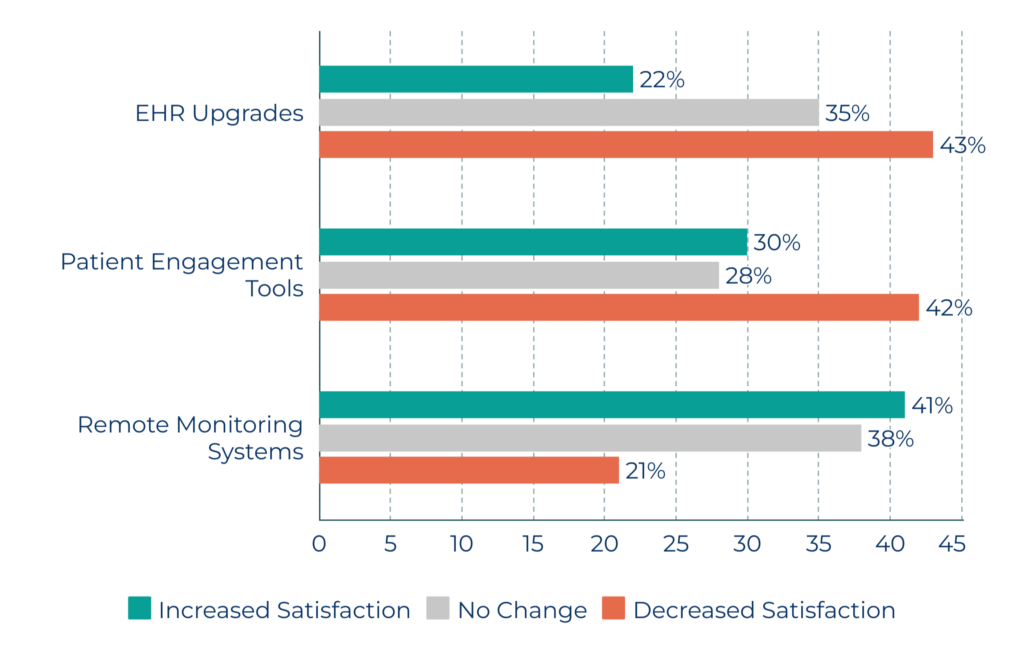
Source: MGMA Practice Tech Satisfaction Survey, 2024
While remote monitoring systems have shown a higher satisfaction rate, most practices report decreased satisfaction after implementing standard EHRs and engagement tools. This is a clear sign: buying tech without a workflow strategy can backfire.
😡 Why Patients Aren’t Impressed, Either
It’s not just clinicians who feel overwhelmed. Patients, too, are struggling to navigate fragmented portals, multiple logins, and notifications that don’t feel human.
Here’s what patients actually care about:
🧠 What Patients Value in Health Tech
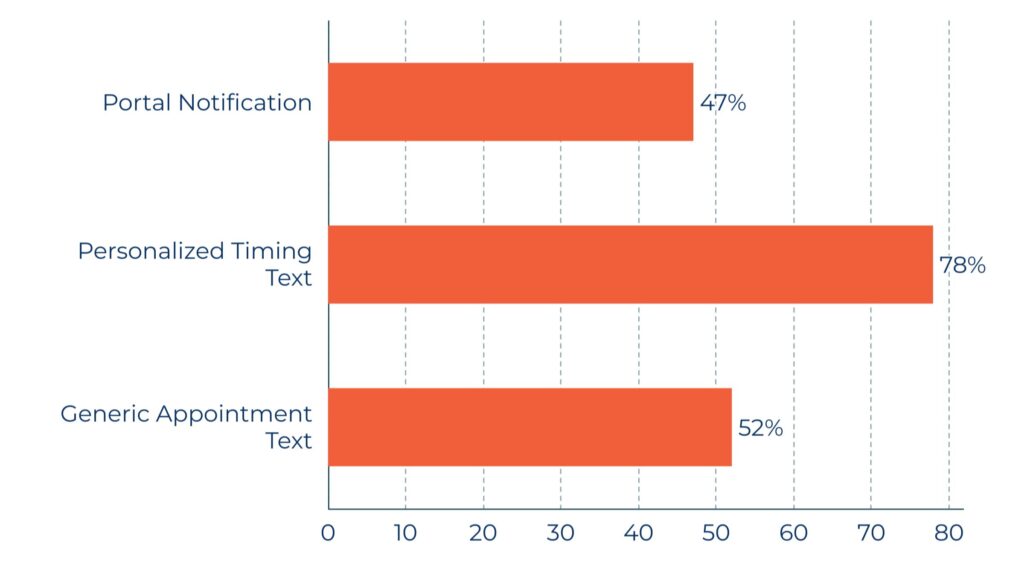
- Source: Rock Health Patient Tech Use Report, 2025
Most patients aren’t asking for fancy AI interfaces or wearable integrations—they want simplicity and connection. If your tools don’t enhance that relationship, they’ll go unused, leading to appointment no-shows, missed follow-ups, and poor chronic care adherence.
🚨 The Real Problem: Implementation, Not Innovation
Here’s the hard truth: most practices don’t have a technology problem.
They have a workflow and engagement problem.
Many teams adopt tools without restructuring their staff responsibilities, communication cadences, or patient education protocols. A patient engagement platform won’t solve anything if your team doesn’t know how to use it—or if patients don’t trust the process.
And most systems lack integration. It’s not unusual for practices to juggle five or more separate platforms, none of which share data in real time. That fragmentation is costing you time, money, and trust.
✅ What Successful Practices Are Doing Differently
Forward-thinking practices have stopped treating technology as a magic bullet. Instead, they are:
- Co-designing tech rollouts with clinicians and staff
Using remote monitoring (RPM) to stay connected between visits—especially for chronic conditions
Consolidating tech tools into a single dashboard or workflow to eliminate redundancies
Focusing on multilingual, accessible platforms that patients want to use
Tracking ROI not just on implementation, but on engagement, no-show reductions, and care outcomes
👣 Final Takeaway
Technology should work for your practice—not create more chaos.
If your tools aren’t easing provider load or improving patient experience, it’s time to rethink your approach. Want help building a smarter remote care strategy that actually works?
